Crohn's disease and actinomycosis - diagnostic difficulties
Adam Bąk1, Elźbieta Poniewierka2, Katarzyna Neubauer1, Szymon Wieczorek1, Michał Jeleń1, Leszek Paradowski Orcid.org 2
+ Pracoviště
Souhrn
We present a case of 42-years old woman, operated in age of 23 because of obstruction, with a suspicion of Crohn's disease. Unexpectedly, postoperative pathological examination revealed actinomycosis and the patient received antibiotics with a good effect. Many years later, according to the recurrence of symptoms of obstruction the patient was operated again. This time, a pathological evaluation of postoperative issues confirmed Crohn's disease, however preoperative tests did now allow to establish the reason of obstruction. Our case shows difficulties in diagnosis of Crohn's disease and actinomycosis. The final diagnosis was established after postoperative pathological examination and all other tests usually helpful in recognition of Crohn's disease were ineffective.
Key words: actinomycosis - Crohn's disease.
INTRODUCTION
According to the recommendations of The European Crohns and Colitis Organisation (ECCO) diagnosis of Crohns disease (CD) is confirmed by "clinical evaluation and a combination of endoscopic, histological, radiological and/or biochemical investigations"(1). Lack of the one diagnostic tool results from the complex disease phenotype: possible location in every part of the digestive tract, occurrence of strictures and fistulas, wide spectrum of intestinal and extraintestinal complications. A significant part of the initial evaluation of patient with suspicion of CD takes microbiological testing to exclude infectious background of diarrhea. Further, bacteria are one of the factors considered in etiopathogenesis of CD(2). Anaerobic bacteria belonging to the Actinomyces family (A. Israeli and A. bovis) is a proofed causative factor of actinomycosis. This saprophytic organism lives in the upper respiratory tract, the entire digestive tract and oral cavity. Abdominal manifestation of actinomycosis encompasses 10-20% of all disease cases. The most common location in digestive tract is ileocaecal segment and appendix(3).
CASE REPORT
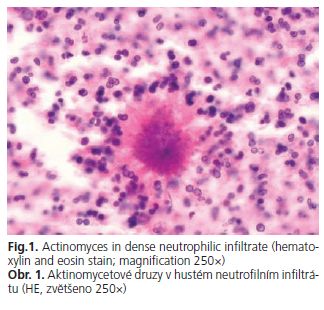
We present case of a 42-years old woman, which was many times hospitalized and treated with antibiotics because of recurring abdominal pain (right lower quadrant) and fever of unknown origin since she was 17. In the age of 23 (1992) the patient was operated because of symptoms of the gastrointestinal obstruction. During the operation the inflammatory infiltration of ileum terminale and enlarged lymph nodes have been found and resected together with an appendix. In spite of clinical and macroscopic suspicion, no features of CD in operative samples were found. Because of persistent symptoms the patient was reoperated and 30 cm long segment of ileum ále was excised. Unexpectedly, a pathological examination revealed presence of Actinomyces in dense neutrophilic infiltrate (Fig. 1). Debecyline for months was administrated. The patient was feeling good for years and in this time was reporting no gastrointestinal symptoms.
In 1997 symptoms of a transient obstruction (attacks of moderate or severe abdominal pain radiating to the right lower quadrant) with fever occurred.
In 2003 the patient was first time hospitalized in Department of Gastroenterology and Hepatology of Medical University in Wroclaw with the initial suspicion of Crohns disease. Biochemical blood investigations, colonoscopy and enteroclysis did not reveal any abnormalities. The patient was effectively treated with ciprofloxacin and considering the past diagnosis of actinomycosis with debecyline. In 2005 the patient was for the second time admitted to this department due to pain in the right lower abdominal quadrant. In colonoscopy a deformation of caecum with multiple scars has been found. Biopsy revealed limfocytary infiltration. The patient was treated with ciprofloxacin with a good effect.
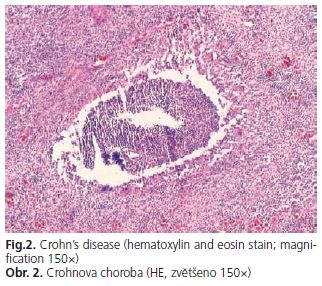
The next exacerbation occurred in 2006. The patient was admitted to the same department as before in severe condition presenting with abdominal pain and fever. Physical examination revealed abdominal tenderness and laboratory test shown high values of inflammatory markers: accelerated erythrocyte sedimentation rate, C-reactive protein, fibrinogen, platelets count and anemia. Microbiological stool tests were negative. Abdominal ultrasonography, computer tomography and barium enema did not show abnormalities. In colonoscopy for a second time deformation of caecum was found. Biopsy was taken for pathological test, that shown chronic inflammation and for microbiological tests (including Actinomycosis), which were negative. The patient was qualified to the surgical treatment. During laparotomy inflammatory tumor of the ileocaecal area with ileal stricture was found. Pathological examination of the excised tumor and ileal segment revealed Crohns disease feature (Fig. 2).
DISCUSSION
Crohns disease and actinomycosis share common clinical feature - eg. symptoms and location of inflammatory changes in the digestive tract. Moreover a complicated postoperative course may appear, what also corresponds to the presented case. Additionally, both conditions can be a diagnostic challenge for a physician. There is no single test sufficient to establish CD diagnosis and many examinations are recommended, including pathological. Tests used for actinomycosis detection are often ineffective. Typical Actinomyces in neutrophilic infiltration occurs only in 40-50 % of cases. Similarly, culture of Actinomyces Israeli is positive only in 30 % of patients(4). This diagnostic problem can be, at least partly, related to wide usage of antibiotics. Furthermore, recent conception of etiopathogenesis of CD includes infectious factor.
We present a case of a coexistence of inflammatory bowel disease and actinomycosis. In described case Crohns disease was diagnosed fourteen years after first diagnosis of actinomycosis. However, in our opinion clinical course suggests that CD was already present when actinomycosis was recognized. Our suggestion, that CD was primary condition is supported by the fact that bacteria causing actinomycosis are saprophytic. Damage of intestinal mucosa in the course of CD facilitate bacteria invasion. Moreover, the primary diagnosis of actinomycosis delayed the diagnosis and proper treatment of inflammatory bowel disease.
The problem of Actinomyces or other bacterial infection as a causative factor of Crohns disease remains open.
REFERENCES
- 1. Stange EF, Travis SPL, Vermeire S i wsp. for the European Crohns and Colitis Organisation (ECCO). European evidence based consensus on the diagnosis and management of Crohns disease: definitions and diagnosis. Gut 2006; 55 (Suppl I): il-il5.
- 2. Sartor RB. Pathogenesis and immune mechanisms of chronic inflammatory bowel diseases. Am J Gastroenterol 1997; 92 (Suppll2): 5S-11S.
- 3. Solecki R, Czupryna A. The case of acute appendicitis with abdominal acinomycosis. Przegl Lek 2001; 58: 466-467.
- 4. Drozdz W. Beben P, Wilczek M. Actinomycosis of large bowel. Przegl Lek 2003; 60: 836-838.
Pro přístup k článku se, prosím, registrujte.
Výhody pro předplatitele
Výhody pro přihlášené