Telemedicine in hepatology – promising solution for our patients?
Daniel Ján Havaj1, Světlana Adamcová Selčanová1, Daniela Žilinčanová1, Ľubomír Skladaný1, Jana Vnenčáková1
+ Affiliation
Summary
Telemedicine refers to the remote provision of health care. Times of crisis like a pandemic and the increasing global burden of liver diseases call for finding innovative healthcare solutions to maintain and improve the standards of care. Provision of health care from a distance based on remote consultations, visits, and monitoring, in addition to standard care, uncovers the potential to improve the quality of care. Despite its challenges, the utilization of telemedicine in many areas of hepatology has been showing promising effects on access, healthcare quality, and cost-effectiveness. We report a case demonstrating the relevant position of telemedicine in the liver transplant decision-making process and our experiences with telehealth in routine clinical praxis.
Keywords
telemedicine, telehealth, teleconsultations, televisits, telemonitoring, liver disease, cirrhosis, liver transplantation, health care quality
Introduction
Digital transformation significantly affects the life of the whole society. Digital technologies are also becoming an important component of the healthcare system. The global burden of chronic liver disease [1] demanding health care including a multidisciplinary approach, regular screening program, care for the chronically critically ill, and a limited supply of hepatologists creates a gap in the cascade and quality of care. Innovative healthcare solutions promise to narrow this gap and improve healthcare quality. Telemedicine, medicine at a distance, opens the opportunity to access high-quality tertiary healthcare anywhere at the time of the patients’ need. It also gives the patient a chance for well-timed intervention in a home setting, without the necessity of hospitalization, based on telemonitoring and televisits. Telehealth holds a promise to revolutionize healthcare [2]. We report the case of a patient who would be contraindicated for liver transplantation due to a fever episode closely preceding the announcement of the suitable donor organ but was granted “staying-active status” owing to the point-of-care analysis of records from telemedicine monitoring.
Case description
Man (36 years) with a history of ulcerative colitis stable on mesalazine and primary sclerotizing cholangitis (PSC) on UDCA treatment was referred in May 2021 to our HEGITO liver unit for liver transplant (LT) consideration. On admission, we ruled out overlap syndrome and other treatable co-factors of advanced chronic liver disease, together with comorbidities that would preclude LT. Ultrasound showed hepatosplenomegaly, circumstantial signs of cirrhosis and small ascites, and elastography by acoustic radiation force impulse imaging proved liver cirrhosis, classified to Child-Pugh B7 and Model for the end-stage liver disease (MELD)-Na 11. The magnetic resonance cholangiopancreatography revealed severe stenosis in the common bile duct and right hepatic duct. The patient was referred for endoscopic retrograde cholangiopancreatography (ERCP) with cholagioscopy which – besides typical PSC picture and biliary stones – detected severe stenosis without clear signs of malignancy. Biliary stones were treated by lithotripsy, and severe stenoses were treated with endoscopic balloon dilatation. Despite the intervention, there was no improvement in the laboratory findings. In July, the patient was re-admitted because of acute cholangitis, treated with intravenous antibiotics, and underwent ERCP with the cleaning of the biliary tree and introduction of a duodenum-biliary drain. Between July and October, the patient was hospitalized further three times for acute cholangitis, during which time further disease progression (MELD-Na 18) was discovered. We indicated liver transplantation and chronic antibiotic treatment. The patient underwent all required examinations and we did not find any contraindications, so in November, he was enrolled on the waiting list for liver transplantation.
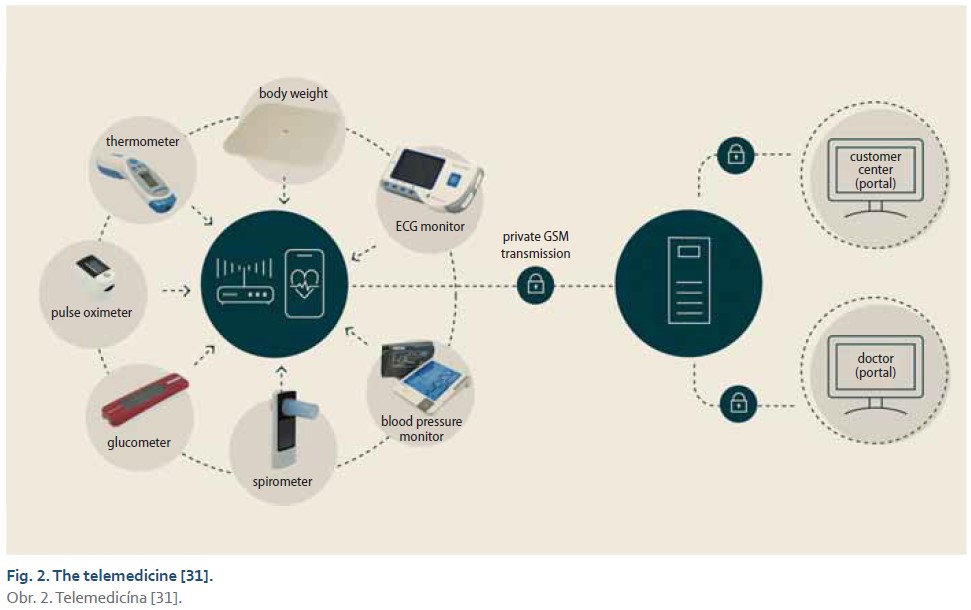
The patient‘s risk profile inspired us to use telemonitoring for early intervention in the case of a flare-up of cholangitis, and assessment of the patient‘s actual condition from the point of infection in the organ allocation process. He signed an informed consent, completed basic education on how to operate the software and devices, and obtained a personal scale, blood pressure monitor, thermometer, pulse oximeter, glucose meter device, and mobile phone with an app gathering data from all the devices and shared them with our center. The App sent automatic alerts regarding critical values, and collected data and alerts were further evaluated by the clinical care team.
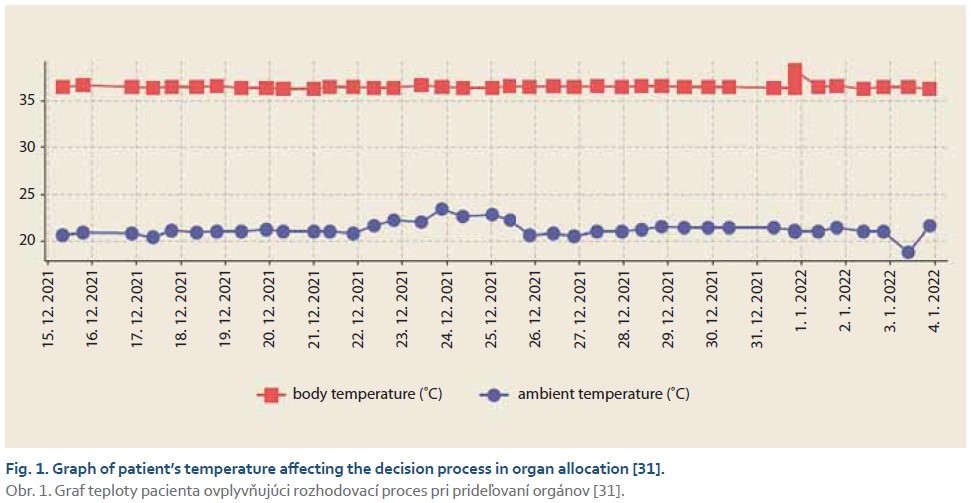
Between November and December, the patient was stable on chronic antibiotic therapy, without any signs of infection according to the acquired data. At the end of December, the telemedicine system showed a single episode of fever without any other pathology in vital signs. We monitored the patient for the next few days and there was no other fever episode. We also contacted him, and he was without any clinical signs of infection. Several days later, a liver transplant became available and in the allocation process, this patient was selected as the most suitable recipient. Usually, the history of fever points to active infection, which is considered a contraindication for liver transplantation. In this case, thanks to telemedicine we were able to distinguish between a coincidental fever episode and uncontrolled infection, and the patient was not disqualified from liver transplantation (Fig. 1).
Discussion
The incidence of liver disease around the world has been increasing for the past ten years. Cirrhosis has been placed within the top 20 causes of death, disability-adjusted life years, and years of life lost worldwide. In Western and industrialized countries, the main etiological factor of cirrhosis is the alcohol-associated liver disease (ALD) and non-alcoholic fatty liver disease (NAFLD), while in Asian countries the most common cause is viral hepatitis B. The autoimmune liver diseases (primary biliary cholangitis, primary sclerotizing cholangitis, and autoimmune hepatitis) are less frequent, despite an increase in their incidence over the past few years, probably due to increased awareness and early detection [1]. In Slovakia, liver diseases rank as the first cause of death in young adults between 25 and 44 years, with alcohol-associated liver disease (ALD) being the leading etiology [3]. These facts reflect the necessity of improvement in awareness of liver diseases and public health and an increase of capacity and quality of health care for these patients.
The pandemic of COVID-19 significantly paralyzed the healthcare system. The social distancing policy restrictions set in Slovakia in March 2020 and the consequent limitation in hepatological tertiary care led to deferment of most planned and on-demand outpatient services, diverting acute hospitalizations to regional lower-rank institutions, and postponing LT except for urgent indications. Liver disease mortality increased significantly during the COVID-19 era according to the Register RH7 [4] and highlighted the importance of time-to-tertiary care as an independent predictor of mortality in patients with acute decompensation of cirrhosis triggered by AH [5]. These findings have become a driving force towards finding the solution for patients without access to hepatological tertiary care, and the application of telemedicine in hepatology could fill the gap in quality of health care [6].
First used in the early 20th century when Willem Einthoven recorded the electrical cardiac signals of hospital patients from the distance of 15 km, telemedicine has rapidly expanded over the past several decades. Application in hepatology was first reported by Thompson in 2015, who used an interactive voice message system for weekly follow-up examinations of patients with recently diagnosed hepatic encephalopathy, variceal hemorrhage, spontaneous bacterial peritonitis, renal failure in the presence of ascites, or ascites requiring paracentesis, and gave them instructions for self-management based on self-reported weakness and weight gain [7]. The World Health Organization defines telemedicine as the provision of healthcare services at a distance with communication conducted between healthcare providers seeking clinical guidance and other supporting healthcare providers (provider-to-provider telemedicine); or conducted between remote healthcare users seeking health services and healthcare providers (client-to-provider telemedicine) [8]. Contemporary telemedicine is based on modern information and communication technologies, which enable interactive communication (synchronous telemedicine) or interaction at different times, the collection of medical data to establish diagnosis and treatment (asynchronous telemedicine). Provision of health care remotely is possible in three different ways of communication. Televisits enable direct real-time contact between the patient and health care provider, like a traditional appointment. Teleconsultations and telementoring represent virtual conferences that allow collaboration between specialists who are available at tertiary centers and support and education from health care providers such as nurses, behavioral therapists, and nutritionists to their patients. A specific type of telemedicine are telemonitoring systems, which acquire information about a patient’s weight and vital functions outside of a conventional clinical setting at a remote location and watch out for signs and symptoms of disease progression. This information gives the caregiver an option for a well-timed therapeutic intervention [1,7,9,10]. The effect of the utilization of telemedicine in the management of heart failure was proven in randomized control trials, systematic reviews, and meta-analyses, which indicated a reduction in mortality, number of emergency hospitalizations, prolonged hospital admissions, and frequent readmissions for heart failure if a patient had remote contact with a health care provider and was involved in the management of their disease. By contrast, publications about telemedicine in hepatology are rare but quickly increasing in amount [11,12]. One of the first projects implementing telemedicine called Extension for Community Healthcare Outcomes (ECHO) in the University of New Mexico Health Sciences Center provided teleconsultations for primary care providers in rural and underserved areas to treat HCV infection. The efficiency of the remote treatment was comparable to the standard of care. Since then, the ECHO project expanded to many parts of the world lacking access to treatment and has shown promising outcomes in the global elimination of HCV infection [9]. Telemedicine has quickly expanded to other segments of hepatology, it has increased access to tertiary care, effective management of patients with hepatocellular carcinoma based on multidisciplinary evaluation by the virtual tumor board, as well as management of general liver disease and pre- and post-liver transplantation care [9,13]. Implementation of telemedicine into the liver transplant program may substantially reduce the time from referral to initial evaluation of liver transplant candidates, shorten the listing time [14], help identify non-candidates for transplantation without the need for additional testing [15], improve care for candidates until liver transplantation [16], and improve outcomes in patients after liver transplantation [17]. Teleconsultations between caregiver and patient have brought a significant benefit through support, education, and early intervention. In patients within the alcoholic liver disease group, the nurse-performed video consultations help prevent relapse, decrease the hospitalization rate and increase the quality of life [18]. The next step forward in telemedicine has become telemonitoring, gathering data about weight, vital signs, and symptoms such as the presence of jaundice, abdominal swelling, weakness, mental conditions, daily sodium intake, need for paracentesis, medication changes, nutrition, and physical activity remotely outside of the clinical environment [19]. Acquired data are processed by mobile phone applications (e. g. Patient Buddy, Platform based on 4G tablets, Encephal App…), and owing to automated alerts and daily evaluation by the clinical care team there is possible early outpatient intervention. The efficiency of this management has been reflected in the reduced burden of cirrhosis complications (hepatic encephalopathy, ascites etc.) [20–22], lower readmission rate [23,24], and higher survival rate [25]. Despite the great potential for improving the efficiency of healthcare access at a reasonable cost and high patient satisfaction [26], there are some challenges. Reimbursement of telemedicine is not covered by national health care insurance and there are also concerns about the quality and accessibility of health care, because of the impossibility of performing clinical examinations, fragmentation of care among multiple providers, and absence of a mutual relationship with a patient (Fig. 2) [9,27].
Telemedicine at the basic level has already been a part of the daily praxis in our transplantation center for a few years. We provide teleconsultation for local healthcare providers about managing patients with ACLD, AD, ACLF, the need for tertiary health care, and evaluating potential liver transplant candidates. We also provide teleconsultation for patients on the waiting list for liver transplantation and patients after liver transplantation.
In August 2021, in cooperation with the Slovak University of Technology in Bratislava and Goldmann Systems s. r. o., we started a pilot project called TELMED in pursuit of providing high-quality tertiary care for patients with advanced chronic liver diseases. We have focused on patients with acute or non-acute decompensation, acute on chronic liver failure, and pre-and post-liver transplantation. The project enrolled 28 patients (18 males and 10 females), aged 26–70, who are registered in cirrhosis registry RH7 (NCT04767945), have access to the Internet, can operate simple technical devices, and gave written informed consent to participate. All patients obtain a personal scale, blood pressure monitor, thermometer, pulse oximeter, glucose meter device, and mobile phone with application gathering data from all devices a sharing them with the caregiver. In the beginning, they got an education on the use of these devices, and during the whole duration of the project, they had on-call technical support. The application of telemonitoring in our patients revealed a potential benefit in several important areas – shortening hospitalization time, decreasing readmission rate, and better evaluation of candidates for liver transplantation.
Conclusion
Advancements in technology and their incorporation into the medical practice have had a significant impact on healthcare quality. The expansion of telemedicine over all segments of medicine has brought to light new ways of improving the outcomes and satisfaction of patients in a cost-effective manner. Despite all the potential benefits of telehealth, the challenging area remains reimbursement and maintaining all ethical aspects of health care [7,9,28].
According to our observation, presented case report, and literature research, we believe that telemedicine’s involvement in managing patients with liver cirrhosis could bridge the gap between the quality, cost, and effectiveness of the treatment. These findings move us closer to the application of telemedicine in a large cohort of patients to assess the efficiency of this modality in routine practice.
ORCID authors
D. J. Havaj ORCID 0000-0001-5979-8326,
S. Adamcová Selčanová ORCID 0000-0001-8181-1937,
J. Vnenčáková ORCID 0000-0001-9125-1662,
Ľ. Skladaný ORCID 0000-0001-5171-3623.
Submitted/Doručené: 15. 2. 2023
Accepted/Prijaté: 12. 3. 2023
Daniel Ján Havaj, MD
2nd Department of Internal Medicine
HEGITO
F. D. Roosevelt University Hospital
Námestie Ludvíka Svobodu 1
975 17 Banská Bystrica
havaj.daniel@gmail.com
To read this article in full, please register for free on this website.
Benefits for subscribers
Benefits for logged users
Literature
1. Asrani SK, Devarbhavi H, Eaton J et al. Burden of liver diseases in the world. J Hepatol 2019; 70(1): 151–171. doi: 10.1016/j.jhep.2018.09.014.
2. Stotts MJ, Grischkan JA, Khungar V. Improving cirrhosis care: The potential for telemedicine and mobile health technologies. World J Gastroenterol 2019; 25(29): 3849–3856. doi: 10.3748/wjg.v25.i29.3849.
3. Zdravotnícka Ročenka Slovenskej Republiky 2018. Národné centrum zdravotníckych infromácií. 2019 [online]. Dostupné z: https: //www.nczisk.sk/aktuality/Pages/Zdravotnicka-rocenka-Slovenskej-republiky-2018.aspx.
4. Skladaný L, Vnencakova J, Havaj DJ et al. Increased mortality and decreased registrations in cirrhosis registry during COVID-19 era. Posters. Hepatology 2020: 72(1): 131–1159. doi: 10.1002/hep.31579.
5. Skladaný L, Jancekova D, Bystrianska N et al. Time-to tertiary care predicts mortality in alcohol-associated hepatitis in patients with cirrhosis. Posters. Hepatology 2021; 74(Suppl 1): 261A–262A. doi: 10.1002/hep.32188.
6. Tapper EB, Asrani SK. The COVID-19 pandemic will have a long-lasting impact on the quality of cirrhosis care. J Hepatol 2020; 73(2): 441–445. doi: 10.1016/j.jhep.2020.04.005.
7. Fung BM, Perumpail M, Patel YA et al. Telemedicine in Hepatology: Current Applications and Future Directions. Liver Transpl 2022; 28(2): 294–303. doi: 10.1002/lt.26293.
8. World Health Organization. Regional Office for the Western Pacific. Implementing telemedicine services during COVID-19: guiding principles and considerations for a stepwise approach. WHO Regional Office for the Western Pacific. 2020 [online]. Dostupné z: https: //apps.who.int/iris/handle/10665/336 862.
9. Piao C, Terrault NA, Sarkar S. Telemedicine: An Evolving Field in Hepatology. Hepatol Commun 2019; 3(5): 3 (5): 716–721. doi: 10.1002/hep4.1340.
10. Serper M, Cubell AW, Deleener ME et al. Telemedicine in Liver Disease and Beyond: Can the COVID-19 Crisis Lead to Action? Hepatology 2020; 72(2): 723–728. doi: 10.1002/hep.31276.
11. Anker SD, Koehler F, Abraham WT. Telemedicine and remote management of patients with heart failure. Lancet 2011; 378: 731–739. doi: 10.1016/S0140-6736(11)61229-4.
12. Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform 2010; 79(11): 736–771. doi: 10.1016/j.ijmedinf.2010.08.006.
13. Choi DT, Sada YH, Sansgiry S et al. Using Telemedicine to Facilitate Patient Communication and Treatment Decision-Making Following Multidisciplinary Tumor Board Review for Patients with Hepatocellular Carcinoma. J Gastrointest Cancer 2022: 1–9. doi: 10.1007/s12029-022-00844-w.
14. John BV, Love E, Dahman B et al. Use of Telehealth Expedites Evaluation and Listing of Patients Referred for Liver Transplantation. Clin Gastroenterol Hepatol 2020; 18(8): 1822–1830.e4. doi: 10.1016/j.cgh.2019.12.021.
15. Konjeti VR, Heuman D, Bajaj JS et al. Telehealth-based Evaluation Identifies Patients Who Are Not Candidates for Liver Transplantation. Clin Gastroenterol Hepatol 2019; 17(1): 207–209.e1. doi: 10.1016/j.cgh.2018.04.048.
16. Ertel AE, Kaiser T, Shah SA. Using telehealth to enable patient-centered care for liver transplantation. JAMA Surg 2015; 150(7): 674–675. doi: 10.1001/jamasurg.2015.0676.
17. Lee TC, Kaiser TE, Alloway R et al. Telemedicine Based Remote Home Monitoring After Liver Transplantation: Results of a Randomized Prospective Trial. Ann Surg 2019; 270(3): 564–572. doi: 10.1097/SLA.0000000000003425.
18. Thygesen GB, Andersen H, Damsgaard BS et al. The effect of nurse performed telemedical video consultations for patients suffering from alcohol-related liver cirrhosis. J Hepatol 2017; 66: S349.
19. Ganapathy D, Acharya C, Lachar J et al. The patient buddy app can potentially prevent hepatic encephalopathy-related readmissions. Liver Int 2017; 37(12): 1843–1851. doi: 10.1111/liv.13494.
20. Rosenblatt R, Yeh J, Gaglio PJ. Long-term management: modern measures to prevent readmission in patients with hepatic encephalopathy. Clin Liver Dis 2020; 24(2): 277–290. doi: 10.1016/j.cld.2020.01.007.
21. Bloom P, Wang T, Marx M et al. A smartphone app to manage cirrhotic ascites among outpatients: feasibility study. JMIR Med Inform 2020; 8(9): e17770. doi: 10.2196/17770.
22. Bloom PP, Ventoso M, Tapper E et al. A telemonitoring intervention for cirrhotic ascites management is cost-saving. Dig Dis Sci 2021; 67(3): 854–862. doi: 10.1007/s10620-021-07013-2.
23. Khungar V, Serper M, Peyton D et al. Use of an Innovative Telehealth Platform to Reduce Readmissions and Enable Patient-Centered Care in Cirrhotic Patients. Hepatology 2017; 66: 94A–95A.
24. Thomson M, Volk M, Kim HM et al. An Automated Telephone Monitoring System to Identify Patients with Cirrhosis at Risk of Re-hospitalization. Dig Dis Sci 2015; 60(12): 3563–3569. doi: 10.1007/s10620-015-3744-3.
25. Su GL, Glass L, Tapper EB et al. Virtual Consultations Through the Veterans Administration SCAN-ECHO Project Improves Survival for Veterans With Liver Disease. Hepatology. 2018; 68(6): 2317–2324. doi: 10.1002/hep.30074.
26. Mauro E, Marciano S, Torres MC et al. Telemedicine Improves Access to Hepatology Consultation with High Patient Satisfaction. J Clin Exp Hepatol 2020; 10(6): 555–562. doi: 10.1016/j.jceh.2020.04.017.
27. Dorsey ER, Topol EJ. State of Telehealth. N Engl J Med 2016; 375: 154–161. doi: 10.1056/NEJMra1601705.
28. Chaet D, Clearfield R, Sabin JE et al. Council on Ethical and Judicial Affairs American Medical Association. Ethical practice in Telehealth and Telemedicine. J Gen Intern Med 2017; 32(10): 1136–1140. doi: 10.1007/s11606-017-4082-2.
29. Goldmann Systems, a. s. Čo je telemedicína? 2023 [online]. Dostupné z: www.telemon.sk.
30. Goldmann Systems, a. s. Meracie prístroje. 2023 [online]. Dostupné z: www.telemon.sk/meracie-pristroje/.